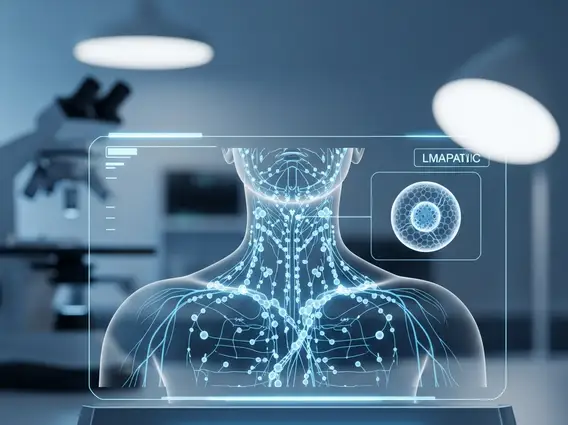
Lymph Node Mapping
Lymph Node Mapping is a critical diagnostic and staging technique used in oncology to determine the spread of cancer. This procedure helps medical professionals make informed decisions regarding treatment plans and prognosis for various types of solid tumors.
Key Takeaways
- Lymph Node Mapping identifies lymph nodes most likely to contain cancer cells.
- The procedure involves injecting a tracer to locate sentinel lymph nodes.
- It is crucial for accurate cancer staging and guiding surgical interventions.
- Minimally invasive, it helps avoid unnecessary extensive lymph node dissection.
- Outcomes significantly influence treatment strategies and patient prognosis.
What is Lymph Node Mapping?
Lymph Node Mapping refers to a specialized medical procedure designed to identify and locate the sentinel lymph node(s) (SLN) – the first lymph node(s) to which cancer cells are most likely to spread from a primary tumor. This technique is invaluable in oncology for accurately staging certain cancers, particularly melanoma, breast cancer, and some gynecological cancers. The purpose of lymph node mapping is to determine if cancer has begun to spread beyond the primary tumor site into the lymphatic system. By identifying the sentinel node, surgeons can assess the risk of regional metastasis without performing a more extensive and potentially morbid lymphadenectomy, which involves removing a larger number of lymph nodes. This targeted approach helps to minimize complications such as lymphedema while still providing crucial information for treatment planning.
The Lymph Node Mapping Procedure
The process of lymph node mapping procedure explained typically involves two main components: injecting a tracer and then surgically locating and removing the sentinel lymph node(s). Before surgery, a radioactive tracer (such as technetium-99m sulfur colloid) or a blue dye, or often both, is injected near the tumor site. The tracer then travels through the lymphatic vessels, mimicking the path cancer cells would take, and accumulates in the sentinel lymph node(s). This allows medical professionals to visualize the lymphatic drainage pathways.
During surgery, a gamma probe (a device that detects radioactivity) is used to locate the “hot” lymph node(s) that have absorbed the radioactive tracer. If a blue dye was also used, the surgeon visually identifies the stained lymph node(s). Once identified, these sentinel lymph nodes are carefully removed and sent to a pathologist for immediate or later examination. The pathologist then analyzes these nodes for the presence of cancer cells. If cancer cells are found in the sentinel node(s), it indicates that the cancer has spread, and further treatment or lymph node dissection may be necessary. If no cancer cells are found, it suggests that the cancer has likely not spread to the regional lymph nodes, potentially allowing for a less aggressive surgical approach and fewer side effects for the patient.
- Tracer Injection: A radioactive substance and/or blue dye is injected near the primary tumor.
- Tracer Migration: The tracer travels through lymphatic channels to the sentinel lymph node(s).
- Detection: A gamma probe and/or visual inspection identifies the sentinel node(s) during surgery.
- Excision: The identified sentinel lymph node(s) are surgically removed.
- Pathological Analysis: The removed nodes are examined under a microscope for cancer cells.
Applications and Outcomes of Lymph Node Mapping
Lymph Node Mapping has revolutionized the management of several cancers by providing a less invasive yet highly accurate method for staging. Its primary application is in cancers where lymphatic spread is a common pathway for metastasis. For instance, in breast cancer, sentinel lymph node biopsy (SLNB) guided by mapping has largely replaced axillary lymph node dissection (ALND) for many patients with early-stage disease, significantly reducing the risk of lymphedema and other complications. According to the American Cancer Society, SLNB is now the standard of care for many women with early-stage breast cancer, with studies showing comparable survival rates to ALND while improving quality of life. Similarly, in melanoma, mapping helps determine the need for complete lymph node dissection, guiding subsequent therapy. The outcomes of this procedure directly impact treatment decisions, including the extent of surgery, the need for adjuvant therapies like chemotherapy or radiation, and overall prognosis. By precisely identifying the status of regional lymph nodes, Lymph Node Mapping enables personalized treatment strategies, optimizing patient care and minimizing unnecessary interventions.