Intratumoral
Intratumoral refers to a method of delivering therapeutic agents directly into a tumor. This approach aims to concentrate treatment at the disease site, potentially enhancing efficacy while minimizing systemic side effects often associated with conventional therapies.
Key Takeaways
- Intratumoral delivery involves injecting therapeutic agents directly into a tumor.
- This method allows for high drug concentrations at the target site, potentially improving local efficacy.
- It can reduce systemic exposure to drugs, thereby mitigating widespread side effects.
- Intratumoral therapy is being explored for various agents, including immunotherapies and oncolytic viruses.
- The approach holds promise for treating localized tumors and modulating the tumor microenvironment.
What is Intratumoral?
Intratumoral is a medical term describing the administration of substances directly into a tumor mass. This method contrasts with systemic delivery, where drugs are circulated throughout the body via the bloodstream. The primary advantage of intratumoral administration is the ability to achieve high concentrations of a therapeutic agent within the tumor, which can be crucial for overcoming drug resistance and maximizing local cytotoxic effects.
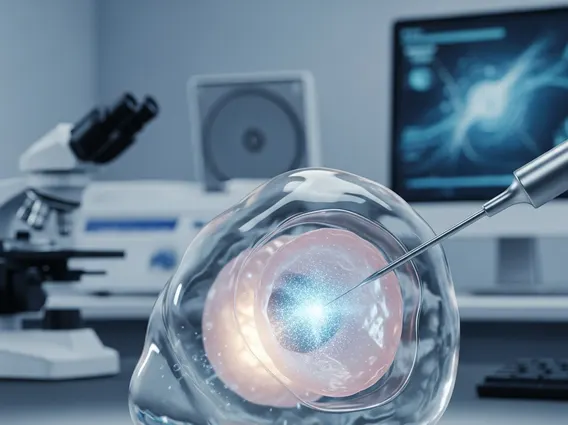
The Intratumoral injection definition specifies a procedure where a needle or catheter is used to precisely deliver a drug or therapeutic agent directly into the cancerous tissue. This localized approach is particularly relevant for solid tumors that are accessible for direct injection. It allows for a targeted attack on cancer cells while potentially sparing healthy surrounding tissues from significant exposure to potent anti-cancer agents, thereby reducing the overall toxicity profile of the treatment.
Intratumoral Therapy: Mechanisms and Applications
Intratumoral therapy explained involves the direct injection of various therapeutic agents into a tumor to elicit a localized anti-cancer response. This strategy is designed to overcome limitations of systemic treatments, such as poor drug penetration into tumor tissue or dose-limiting systemic toxicities. By delivering agents directly to the tumor, higher concentrations can be achieved at the site of disease, which can be particularly effective for agents with narrow therapeutic windows or those that require high local concentrations to be effective.
The Intratumoral drug delivery mechanism relies on the physical introduction of the therapeutic agent into the tumor mass. Once injected, the agent can exert its effects directly on tumor cells and the surrounding tumor microenvironment. This mechanism is particularly beneficial for:
- Immunotherapies: Agents like checkpoint inhibitors or cytokines can be delivered directly to activate local immune responses within the tumor, potentially turning “cold” tumors into “hot” ones.
- Oncolytic Viruses: These viruses are engineered to selectively infect and replicate within cancer cells, leading to their lysis and the release of tumor antigens, which can further stimulate an anti-tumor immune response.
- Chemotherapeutic Agents: Direct delivery can increase local drug exposure, potentially overcoming resistance mechanisms and reducing systemic side effects compared to intravenous administration.
- Gene Therapies: Introducing genes that promote tumor suppression or enhance drug sensitivity directly into cancer cells.
Intratumoral therapy holds significant promise in oncology, especially for localized tumors or as a strategy to prime the immune system for a broader systemic response. Clinical trials are exploring its application across various cancer types, including melanoma, head and neck cancers, and breast cancer, aiming to refine delivery techniques and optimize therapeutic outcomes.