Cordectomy
Cordectomy is a specialized surgical procedure that involves the partial or complete removal of a vocal cord. This intervention is primarily undertaken to address specific conditions affecting the larynx, most notably early-stage malignant tumors of the vocal cords.
Key Takeaways
- Cordectomy is the surgical removal of part or all of a vocal cord, primarily for early-stage vocal cord cancer.
- The procedure can be performed using various techniques, including endoscopic and open surgical approaches.
- Recovery typically involves a period of voice rest and may require subsequent voice therapy to optimize vocal function.
- Benefits include high rates of disease control for appropriate cases, while potential risks involve changes in voice quality.
- The extent of vocal cord removal dictates the impact on voice and swallowing functions.
What is Cordectomy?
Cordectomy refers to the surgical excision of a portion or the entirety of one or both vocal cords. This procedure is a critical treatment option within otolaryngology, particularly in oncology, for managing lesions and early-stage cancers of the glottis (the vocal cords and the space between them). The goal of this cordectomy surgery is to remove diseased tissue while preserving as much healthy vocal cord structure as possible to maintain voice and swallowing functions.
The decision to perform a cordectomy is made after careful evaluation, often involving laryngoscopy and biopsy, to accurately diagnose the condition. The extent of the removal, classified by different types (e.g., Type I to Type VI), depends on the size, location, and depth of the lesion. For instance, a Type I cordectomy involves only the superficial layer, while more extensive types involve deeper tissues or the entire vocal cord.
Cordectomy Procedure and Recovery
The Cordectomy procedure and recovery process are tailored to the individual patient’s condition and the surgical approach utilized. Modern techniques for vocal cord removal surgery details often involve minimally invasive endoscopic approaches, where instruments are passed through the mouth to access the larynx. This allows for precise removal of the affected tissue with minimal external incisions. In some cases, an open surgical approach may be necessary for larger or more complex lesions.
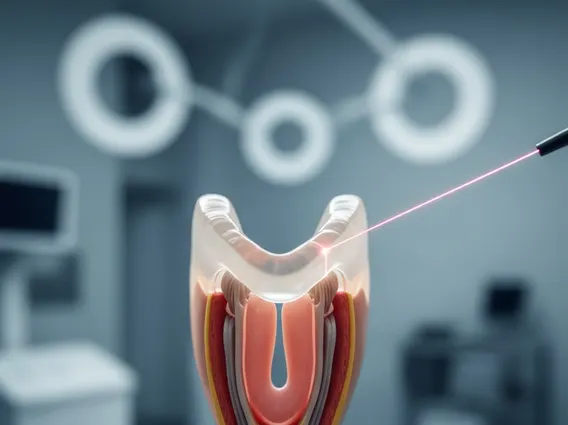
During an endoscopic cordectomy, a microscope or endoscope provides magnified views, enabling the surgeon to use lasers or micro-instruments to resect the vocal cord tissue. This precision helps in achieving clear margins while minimizing damage to surrounding healthy tissue. Post-operatively, patients typically experience a period of voice rest, which is crucial for healing and preventing complications. The duration of voice rest varies but can range from a few days to several weeks.
Recovery from cordectomy also often includes voice therapy, which helps patients adapt to any changes in their voice and learn techniques to improve vocal quality and function. Swallowing difficulties are generally temporary but can occur depending on the extent of tissue removed. Pain management and monitoring for signs of infection are also standard components of the recovery phase.
Different types of cordectomy are defined by the extent of tissue removed:
- Type I (Subepithelial Cordectomy): Removal of the superficial layer of the vocal cord.
- Type II (Subligamental Cordectomy): Excision of the epithelium and superficial lamina propria.
- Type III (Transmuscular Cordectomy): Removal of the entire vocal cord, including the vocalis muscle.
- Type IV (Total Cordectomy): Complete removal of the vocal cord from the anterior commissure to the vocal process.
- Type V (Extended Cordectomy): Involves removal of the vocal cord and adjacent structures, such as the anterior commissure or arytenoid.
Risks and Benefits of Cordectomy
When considering Cordectomy risks and benefits, it is important to weigh the potential for disease eradication against the possible impact on vocal function. The primary benefit of cordectomy, especially for early-stage glottic cancer, is its high efficacy in achieving local control and cure. For T1a glottic cancers, cordectomy can achieve cure rates exceeding 90%, comparable to radiation therapy, as indicated by various studies in oncology literature.
However, like any surgical procedure, cordectomy carries potential risks. The most common and significant risk is a change in voice quality. Patients may experience hoarseness, breathiness, reduced vocal projection, or difficulty sustaining pitch, depending on the amount of vocal cord tissue removed and the healing process. Other potential risks include temporary or, rarely, persistent swallowing difficulties (dysphagia), aspiration (food or liquid entering the airway), bleeding, infection, and airway obstruction.
The decision to undergo cordectomy is made in consultation with a multidisciplinary team, considering the patient’s overall health, the nature of the lesion, and their vocal demands. The aim is always to achieve the best possible oncological outcome while striving to preserve the patient’s quality of life, including their ability to speak and swallow effectively.
