Collecting Duct
The collecting duct is a vital component of the kidney’s intricate filtration system, playing a crucial role in the final adjustments of urine composition. It is essential for maintaining the body’s fluid balance, electrolyte levels, and acid-base homeostasis.
Key Takeaways
- The Collecting Duct is the final segment of the renal tubule, responsible for fine-tuning urine concentration.
- Its primary functions include reabsorbing water, sodium, and bicarbonate, and secreting potassium and hydrogen ions.
- The activity of the Collecting Duct is heavily regulated by hormones like antidiuretic hormone (ADH) and aldosterone.
- Dysfunction of the Collecting Duct can lead to various conditions, including disorders of water balance and acid-base regulation.
What is the Collecting Duct? Anatomy and Physiology
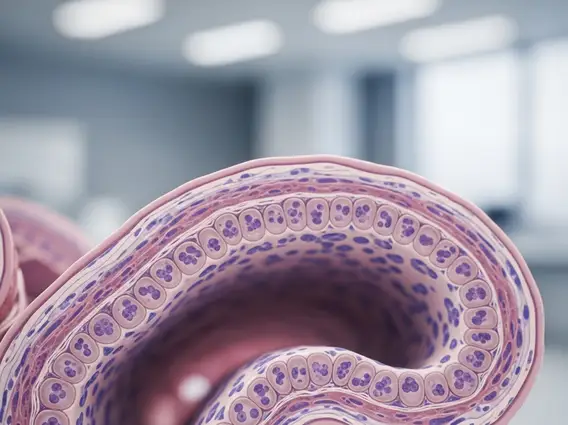
The Collecting Duct is a critical part of the kidney’s excretory system, serving as the final segment of the renal tubule where urine concentration and composition are precisely regulated. Understanding the collecting duct anatomy physiology reveals its unique structure and cellular makeup, which enable its diverse functions.
Located primarily in the renal medulla, the collecting ducts receive filtrate from multiple nephrons. These ducts merge to form larger papillary ducts, which eventually empty into the renal pelvis. The walls of the collecting duct are lined with two main types of cells: principal cells and intercalated cells. Principal cells are primarily involved in water and sodium reabsorption and potassium secretion, while intercalated cells play a significant role of collecting duct in kidney acid-base balance by secreting or reabsorbing hydrogen and bicarbonate ions.
Key Functions and Role of the Collecting Duct
The primary function of collecting duct is to fine-tune the reabsorption of water and electrolytes, ensuring the body maintains appropriate fluid volume and blood pressure. Its activities are tightly regulated by hormonal signals, allowing the kidneys to adapt to varying physiological demands.
The specific functions of the collecting duct include:
- Water Reabsorption: Under the influence of antidiuretic hormone (ADH), principal cells become permeable to water, allowing water to be reabsorbed from the filtrate into the hypertonic medullary interstitium. This process is crucial for producing concentrated urine and preventing dehydration.
- Sodium Reabsorption: Aldosterone, a hormone from the adrenal cortex, stimulates principal cells to reabsorb sodium ions, which often leads to water reabsorption and contributes to blood pressure regulation.
- Potassium Secretion: Principal cells also secrete potassium ions into the filtrate, a mechanism vital for maintaining potassium balance in the body.
- Acid-Base Balance: Intercalated cells regulate the body’s pH by secreting hydrogen ions (acid) or reabsorbing bicarbonate ions (base), depending on the body’s needs. This precise control prevents acidosis or alkalosis.
These coordinated actions highlight the indispensable role of collecting duct in kidney function, ensuring the stability of the internal environment.
Conditions Affecting the Collecting Duct
Dysfunction of the collecting duct can lead to various clinical conditions, collectively known as collecting duct diseases. These disorders often manifest as imbalances in fluid, electrolyte, or acid-base regulation, reflecting the duct’s critical physiological roles.
Several conditions can impair the normal functioning of the collecting duct, leading to significant health issues. These conditions can arise from genetic defects, hormonal imbalances, or structural damage to the kidney.
| Condition | Primary Impact on Collecting Duct | Key Consequence |
|---|---|---|
| Nephrogenic Diabetes Insipidus | Principal cells fail to respond to ADH | Inability to concentrate urine, leading to excessive urination and thirst |
| Renal Tubular Acidosis (Type 1 & 4) | Impaired hydrogen ion secretion or aldosterone resistance in intercalated cells | Metabolic acidosis (Type 1) or hyperkalemia and acidosis (Type 4) |
| Sickle Cell Nephropathy | Damage to the renal medulla and collecting ducts due to sickling | Reduced ability to concentrate urine, leading to nocturia and polyuria |
| Polycystic Kidney Disease | Cyst formation within the collecting ducts and other nephron segments | Progressive decline in kidney function, impaired urine concentration |
Early diagnosis and management of these conditions are crucial to prevent long-term complications and preserve kidney health.
