Borderline Breast Disease
Borderline breast disease refers to a group of breast conditions that are not cancerous but carry an increased risk of developing into invasive breast cancer over time. Understanding these conditions is crucial for appropriate monitoring and management.
Key Takeaways
- Borderline Breast Disease encompasses several non-cancerous conditions that elevate future breast cancer risk.
- These conditions are typically identified through biopsies performed for abnormal mammogram findings or palpable lumps.
- Common types include atypical ductal hyperplasia (ADH), atypical lobular hyperplasia (ALH), and lobular carcinoma in situ (LCIS).
- Management often involves close surveillance, and in some cases, surgical excision or risk-reducing medications may be considered.
- Regular follow-up with a healthcare provider is essential for individuals diagnosed with borderline breast disease.
What is Borderline Breast Disease?
Borderline Breast Disease is a classification used for certain breast lesions that exhibit features between benign (non-cancerous) and malignant (cancerous) conditions. These lesions are not invasive cancers themselves, but their presence indicates an elevated risk for developing invasive breast cancer in the future. The term encompasses several specific pathological diagnoses, each with varying degrees of associated risk.
These conditions are often characterized by abnormal cell growth patterns within the breast ducts or lobules. While they do not invade surrounding tissues like cancer, their atypical cellular architecture signals a predisposition to malignant transformation. Examples include atypical ductal hyperplasia (ADH), atypical lobular hyperplasia (ALH), and lobular carcinoma in situ (LCIS).
Borderline Breast Disease: Symptoms, Diagnosis, and Risk Factors
Individuals with borderline breast disease symptoms and diagnosis typically do not experience specific symptoms directly attributable to these lesions. Most cases are discovered incidentally during routine mammograms or when a biopsy is performed for other reasons, such as a suspicious lump or an abnormal finding on imaging. When a suspicious area is identified, a biopsy is necessary to obtain tissue for pathological examination.
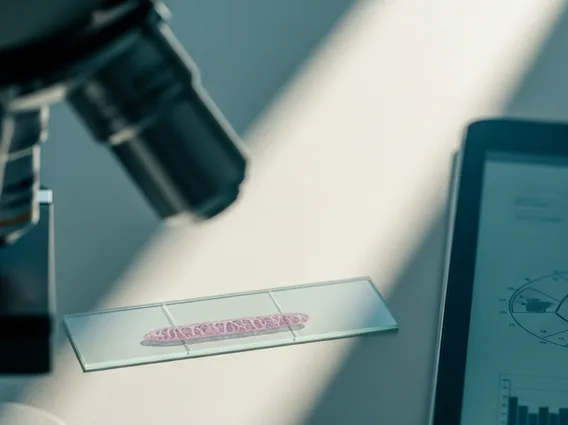
Diagnosis involves a pathologist examining the tissue sample under a microscope to identify the characteristic cellular changes. Imaging techniques like mammography, ultrasound, and MRI play a crucial role in initial detection and guiding biopsies, but a definitive diagnosis relies on histopathological analysis.
Several factors contribute to borderline breast disease risk factors, increasing an individual’s likelihood of developing these conditions and subsequently, breast cancer. These include:
- Family History: A strong family history of breast cancer, particularly in first-degree relatives.
- Genetic Mutations: Presence of certain genetic mutations, such as BRCA1 or BRCA2, although these are more directly linked to invasive cancer risk.
- Age: Risk generally increases with age, particularly after 35.
- Reproductive History: Factors like early menarche, late menopause, or never having given birth.
- Previous Breast Biopsies: A history of previous benign breast conditions, especially those with atypical features.
- Hormone Exposure: Prolonged exposure to estrogen, either endogenous or exogenous (e.g., certain hormone replacement therapies).
It is important to note that having one or more risk factors does not guarantee the development of borderline breast disease or cancer, but it warrants closer monitoring.
Treatment Options for Borderline Breast Lesions
The management of borderline breast lesions treatment options varies depending on the specific diagnosis and individual risk profile. The primary goal is to reduce the risk of progression to invasive breast cancer and ensure early detection if cancer does develop. For many borderline lesions, such as atypical ductal hyperplasia (ADH) or atypical lobular hyperplasia (ALH), complete surgical excision of the lesion is often recommended to ensure no higher-risk lesions are present nearby and to confirm the diagnosis. This is because a biopsy might sometimes underestimate the extent or nature of the abnormality.
Following excision, surveillance is a cornerstone of management. This typically involves more frequent clinical breast exams and imaging (mammograms, and sometimes MRI) than for the general population. For individuals with a significantly elevated risk, particularly those with lobular carcinoma in situ (LCIS) or extensive ADH, risk-reducing medications such as tamoxifen or raloxifene may be discussed. These medications can help lower the risk of developing future breast cancer. In very rare, high-risk cases, prophylactic mastectomy might be considered, though this is less common for borderline lesions alone and is usually reserved for individuals with very high genetic risk factors.
