Cone Biopsy
A cone biopsy is a surgical procedure used to diagnose and treat abnormal cells on the cervix. This article will explain the procedure, what to expect during recovery, potential risks and benefits, and how to interpret your results.

Key Takeaways
- A cone biopsy is a diagnostic and therapeutic procedure for cervical abnormalities.
- It involves removing a cone-shaped tissue sample from the cervix for examination.
- Recovery typically involves several weeks of rest and avoiding certain activities.
- The procedure carries both potential risks, like bleeding or infection, and significant benefits in preventing cervical cancer.
- Understanding your biopsy results is crucial for determining subsequent treatment or monitoring.
What is Cone Biopsy?
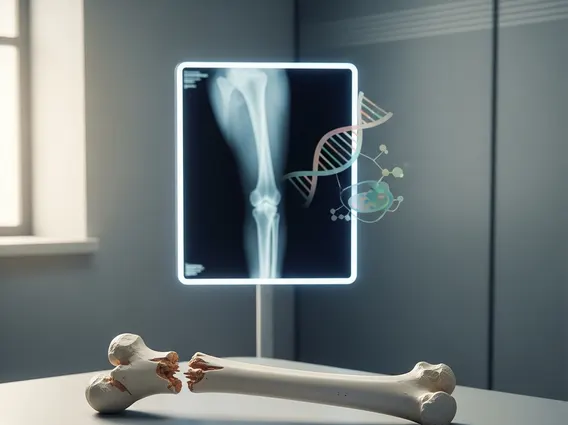
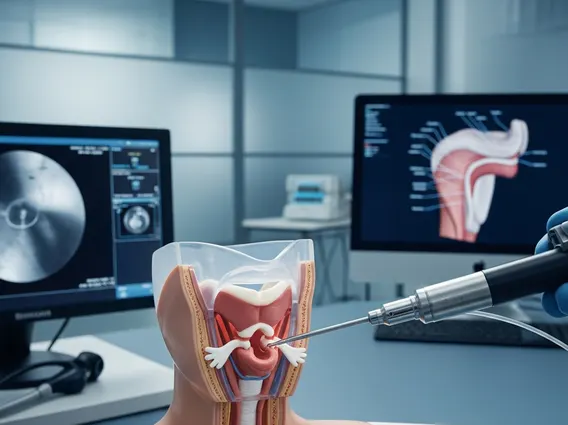
A cone biopsy, also known as a conization, is a surgical procedure that removes a cone-shaped piece of tissue from the cervix. This tissue is then sent to a laboratory for microscopic examination. Its primary goal is to diagnose and, in many cases, treat precancerous conditions or early-stage cervical cancer.
The Procedure Explained
A cone biopsy procedure is typically performed when abnormal cervical screening results, such as an abnormal Pap test or HPV test, indicate high-grade cervical dysplasia or adenocarcinoma in situ. Performed under general or regional anesthesia, the surgeon removes the abnormal tissue using a scalpel (cold knife conization), a laser, or a loop electrosurgical excision procedure (LEEP). The aim is to remove all abnormal cells while preserving healthy cervical tissue. The removed tissue includes the transformation zone, where most cervical cancers originate.
Recovery, Risks, and Benefits
Undergoing any medical procedure comes with questions about the aftermath and potential outcomes. A cone biopsy is no exception, with specific considerations for healing and potential complications.
Managing Recovery and Tips
The cone biopsy recovery time and tips are vital for a smooth healing process. Most individuals can expect a recovery period of approximately 4 to 6 weeks. During this time, it is common to experience vaginal discharge, light bleeding, or spotting. To facilitate healing and prevent complications, healthcare providers typically recommend:
- Avoiding strenuous activities, heavy lifting, and douching.
- Refraining from sexual intercourse.
- Not using tampons; only sanitary pads should be used.
- Taking over-the-counter pain relievers for mild discomfort.
- Following all post-operative instructions provided by your doctor.
It is important to contact your doctor if you experience heavy bleeding, fever, severe pain, or foul-smelling discharge.
Potential Risks and Advantages
When considering the risks and benefits of cone biopsy, it’s important to weigh both sides. Potential risks, though generally low, can include bleeding, infection, cervical stenosis (narrowing of the cervix), or, in rare cases, an increased risk of premature birth in future pregnancies. According to the American College of Obstetricians and Gynecologists (ACOG), while there is a slight increase in the risk of preterm birth, the benefits of treating precancerous lesions often outweigh this risk, especially for high-grade abnormalities.
The primary benefit is its dual role as both a diagnostic and therapeutic tool. It provides a definitive diagnosis by allowing pathologists to examine the full extent of the abnormal tissue, including the margins. Therapeutically, it can remove all precancerous cells, thereby preventing their progression to invasive cervical cancer. This preventive aspect is a significant advantage, potentially saving lives.
Understanding Your Results
Receiving the pathology report after a cone biopsy can be a source of anxiety, making understanding cone biopsy results a critical step in your healthcare journey.
The pathologist’s report will detail the type and grade of abnormal cells found, such as cervical intraepithelial neoplasia (CIN) or adenocarcinoma in situ (AIS). Crucially, the report will also specify the status of the “margins,” which are the edges of the removed tissue.
- Negative or Clear Margins: This indicates that no abnormal cells were found at the edges of the removed tissue, suggesting that all precancerous cells have likely been excised.
- Positive or Involved Margins: This means that abnormal cells were found at the edges, indicating that some abnormal tissue might still remain on the cervix. This may necessitate further monitoring or treatment.
Your healthcare provider will explain the results thoroughly and discuss the appropriate next steps, which could range from continued surveillance with regular Pap tests and HPV tests to additional procedures, depending on the findings and your individual circumstances.