Biliary Bypass
Biliary bypass is a surgical procedure designed to reroute the flow of bile when the natural drainage system is obstructed. This intervention is crucial for patients experiencing blockages that can lead to severe health complications.
Key Takeaways
- Biliary bypass surgery creates a new pathway for bile to flow around an obstruction.
- It is primarily performed to alleviate symptoms caused by blockages in the bile ducts, often due to tumors or strictures.
- The procedure involves connecting a bile duct or the gallbladder directly to the small intestine.
- Recovery typically involves a hospital stay, pain management, and gradual dietary adjustments.
- Successful bypass can significantly improve quality of life by resolving jaundice and reducing pain.
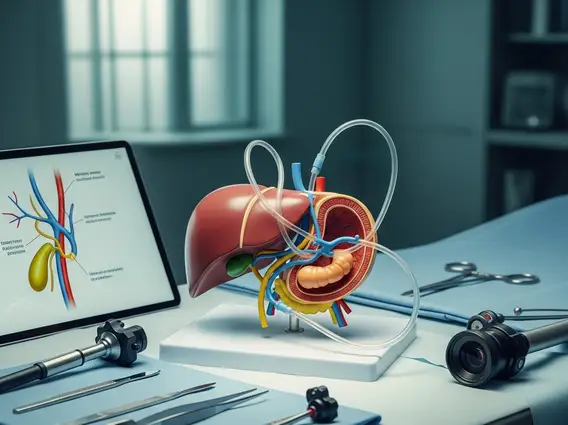
What is Biliary Bypass?
A biliary bypass is a surgical intervention aimed at restoring the normal flow of bile from the liver and gallbladder into the small intestine. When the bile ducts become blocked, bile can back up, leading to serious conditions such as jaundice, infection, and liver damage. Understanding what is biliary bypass surgery involves recognizing it as a reconstructive procedure that creates an alternative route for bile drainage, bypassing the obstructed segment.
This procedure is a critical solution for patients whose bile ducts are impassable due to various medical conditions. By creating a new connection, often to the jejunum (a part of the small intestine), the surgery helps to relieve pressure, reduce symptoms, and prevent further complications associated with bile stasis.
Reasons for Biliary Bypass Surgery
There are several compelling reasons for biliary bypass surgery, primarily stemming from conditions that cause irreversible obstruction of the bile ducts. These obstructions can lead to debilitating symptoms and life-threatening complications if left untreated. Common indications include:
- Pancreatic Cancer: Tumors in the head of the pancreas are a frequent cause of bile duct compression, leading to jaundice. A bypass can relieve this obstruction.
- Bile Duct Tumors: Cancers originating within the bile ducts (cholangiocarcinoma) often necessitate bypass surgery to restore flow.
- Benign Bile Duct Strictures: Non-cancerous narrowing of the bile ducts, often resulting from inflammation, injury during previous surgery, or chronic pancreatitis, can also cause blockages.
- Severe Gallstones: In rare cases, large or impacted gallstones can obstruct the common bile duct, and if endoscopic removal is not feasible, a bypass may be considered.
According to the American Cancer Society, pancreatic cancer is a significant cause of biliary obstruction, highlighting the importance of procedures like biliary bypass in managing its complications and improving patient comfort.
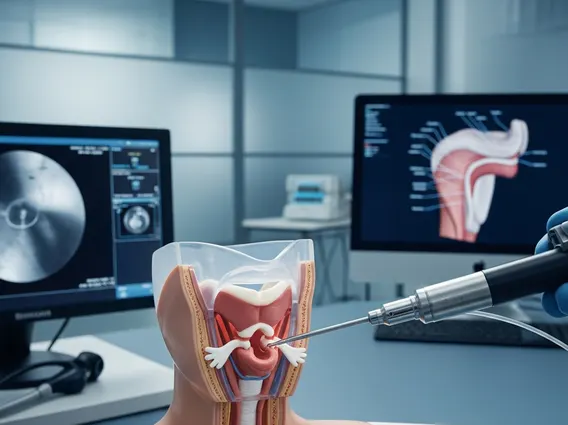
The Biliary Bypass Procedure Explained
The biliary bypass procedure explanation typically involves a complex surgical operation performed under general anesthesia. The specific technique chosen depends on the location and nature of the obstruction, as well as the patient’s overall health. The primary goal is to create a new connection between a bile-carrying structure (either a bile duct or the gallbladder) and a segment of the small intestine, usually the jejunum.
Common types of biliary bypass include:
- Choledochojejunostomy: This involves connecting the common bile duct directly to the jejunum.
- Hepaticojejunostomy: Used when the obstruction is higher up, closer to the liver, connecting one of the hepatic ducts to the jejunum.
- Cholecystojejunostomy: In some cases, if the gallbladder is healthy and the obstruction is distal to the cystic duct, the gallbladder itself can be connected to the jejunum.
The surgery can be performed using traditional open surgery (involving a larger incision) or, in some suitable cases, laparoscopically (minimally invasive with smaller incisions and specialized instruments). The surgeon carefully identifies the obstructed area, isolates the healthy bile duct or gallbladder, and then sutures it to a loop of the small intestine, ensuring a watertight connection to allow bile to drain freely.
Biliary Bypass Recovery and Aftercare
Receiving comprehensive biliary bypass recovery information is vital for patients and their families. The recovery period typically begins with a hospital stay, which can range from several days to a week or more, depending on the complexity of the surgery and the patient’s general health. During this time, pain management is a priority, often involving intravenous medications that are gradually transitioned to oral pain relievers.
Patients will initially be on a liquid diet, progressing slowly to soft foods and then a regular diet as their digestive system recovers. Monitoring for complications such as infection, leakage from the surgical site, or persistent jaundice is crucial. Post-discharge care includes:
- Wound Care: Keeping the incision site clean and dry to prevent infection.
- Activity Restrictions: Avoiding heavy lifting and strenuous activities for several weeks to allow internal healing.
- Dietary Adjustments: Some patients may need to follow a low-fat diet for a period to aid digestion, as bile flow may be altered.
- Follow-up Appointments: Regular visits with the surgeon and oncologist (if cancer-related) are essential to monitor recovery, assess the success of the bypass, and manage any underlying conditions.
Full recovery can take several weeks to a few months. Adherence to medical advice and lifestyle adjustments are key to achieving the best possible long-term outcomes and improving the patient’s quality of life.