Diagnosis, Screening, and Early Detection of Primary CNS Lymphoma
Primary Central Nervous System Lymphoma (PCNSL) is a rare and aggressive form of non-Hodgkin lymphoma that originates in the brain, spinal cord, or eyes. Understanding its diagnosis, screening, and the critical importance of early detection is paramount for effective management and improved patient outcomes.
Key Takeaways
- Early detection primary CNS lymphoma is crucial for improving patient prognosis and treatment efficacy.
- Initial symptoms of PCNSL are often non-specific, including neurological deficits and cognitive changes, making diagnosis challenging.
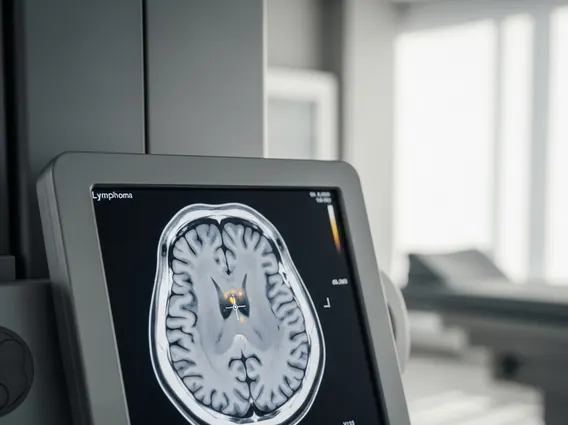
- Primary CNS lymphoma diagnosis methods rely on advanced imaging (MRI) and definitive tissue biopsy or cerebrospinal fluid analysis.
- Universal primary cns lymphoma screening is not standard; screening efforts focus on high-risk populations, such as immunocompromised individuals.
- Differentiating PCNSL from other neurological conditions requires a comprehensive diagnostic approach due to overlapping symptoms and imaging findings.
Recognizing Early Indicators of Primary CNS Lymphoma
Recognizing the Symptoms and early signs of CNS lymphoma is often challenging due to their non-specific nature, frequently mimicking other neurological conditions. These indicators typically develop over weeks to months, making prompt medical evaluation essential.
Common Neurological Symptoms
Patients with PCNSL often present with a range of neurological symptoms that reflect the location and size of the tumor within the central nervous system. These can include:
- Headaches: Persistent or worsening headaches are a common complaint, though they are also associated with many other conditions.
- Seizures: New-onset seizures, either focal or generalized, can be an early indicator, particularly if there’s no prior history of epilepsy.
- Focal Neurological Deficits: Weakness or numbness on one side of the body, visual disturbances (such as blurred vision or double vision), speech difficulties (aphasia), or problems with coordination and balance. These deficits depend on the specific brain region affected.
Cognitive and Behavioral Changes
Beyond physical symptoms, PCNSL can also manifest through subtle yet significant changes in cognitive function and behavior. These changes are often insidious and may initially be attributed to other factors, delaying the Early detection primary CNS lymphoma.
- Memory Loss: Difficulty recalling recent events or learning new information.
- Personality Changes: Increased irritability, apathy, or changes in mood and behavior that are uncharacteristic for the individual.
- Confusion and Disorientation: Problems with concentration, difficulty performing routine tasks, or general confusion about time and place.
According to the National Cancer Institute, these neurological and cognitive symptoms are present in over 70% of PCNSL patients at diagnosis, underscoring the importance of thorough investigation when such signs emerge, especially in at-risk individuals.
Primary CNS Lymphoma Diagnosis Methods
A definitive primary cns lymphoma diagnosis requires a combination of advanced imaging and pathological confirmation. The diagnostic process is crucial for distinguishing PCNSL from other brain lesions and initiating appropriate treatment.
Advanced Imaging Techniques (MRI, CT)
Initial evaluation for suspected PCNSL typically begins with neuroimaging. Magnetic Resonance Imaging (MRI) with contrast is considered the most sensitive imaging modality for detecting brain lesions associated with PCNSL. It can reveal characteristic features such as periventricular lesions, often with homogeneous enhancement after contrast administration.
Computed Tomography (CT) scans may also be used, particularly in emergency settings, but they are generally less sensitive than MRI for detecting subtle lesions. Both techniques help in identifying the location and extent of the tumor, guiding subsequent diagnostic steps. Understanding primary CNS lymphoma diagnosis often starts with these visual clues, though they are not conclusive on their own.
Biopsy and Cerebrospinal Fluid Analysis
The gold standard for confirming a primary cns lymphoma diagnosis is histological examination of tissue. This is typically achieved through a stereotactic brain biopsy, where a small sample of the suspicious lesion is surgically removed and analyzed by a neuropathologist. This procedure allows for definitive identification of lymphoma cells and classification of the specific type of lymphoma.
Cerebrospinal fluid (CSF) analysis is another vital component of the diagnostic workup. A lumbar puncture is performed to collect CSF, which is then examined for the presence of malignant cells (cytology), elevated protein levels, and specific markers via flow cytometry or molecular studies. CSF analysis is particularly important for detecting leptomeningeal involvement, which can impact staging and treatment decisions. These are among the key Primary CNS lymphoma diagnosis methods.
In some cases, especially when brain biopsy is not feasible or safe, vitreous biopsy (for ocular lymphoma) or even bone marrow biopsy might be considered if systemic lymphoma is suspected to rule out secondary CNS involvement.
Screening for Primary CNS Lymphoma
Unlike some more common cancers, there are no universal Screening guidelines for CNS lymphoma for the general population. This is primarily due to the rarity of the disease and the lack of cost-effective, non-invasive screening tests that could identify PCNSL before symptoms appear.
Current Screening Approaches
Currently, there isn’t a standardized or routine primary cns lymphoma screening program. The focus remains on prompt investigation of individuals presenting with suggestive neurological symptoms. Research is ongoing into potential biomarkers in blood or CSF that could indicate the presence of PCNSL, but these are not yet part of routine clinical practice for screening purposes. Therefore, the concept of Best screening tests for CNS lymphoma is largely theoretical for the general public.
Target Populations for Screening
While universal screening is not practical, certain populations are at a higher risk for developing PCNSL, making vigilance and a lower threshold for diagnostic investigation crucial. These target populations include:
- Immunocompromised Individuals: People with HIV/AIDS, particularly those with low CD4 counts, have a significantly increased risk of PCNSL. For this group, any new neurological symptom warrants immediate and thorough investigation.
- Organ Transplant Recipients: Patients on long-term immunosuppressive therapy following organ transplantation also have an elevated risk. Regular monitoring and prompt evaluation of neurological changes are critical.
- Individuals with Primary Immunodeficiency Syndromes: Certain rare genetic conditions that compromise the immune system can also increase PCNSL risk.
For these high-risk groups, clinicians maintain a heightened awareness, and diagnostic imaging or CSF analysis may be performed more readily when symptoms arise, effectively serving as a form of targeted surveillance rather than broad screening.
Differentiating PCNSL from Other Conditions
One of the significant challenges in achieving a timely primary cns lymphoma diagnosis lies in its differentiation from a myriad of other neurological conditions. The symptoms and imaging characteristics of PCNSL can often mimic those of more common diseases, leading to potential delays in diagnosis.
Challenges in Differential Diagnosis
The non-specific nature of PCNSL symptoms means they can overlap with those of various other conditions, including:
- Other Brain Tumors: Gliomas, metastases from systemic cancers, and other primary brain tumors can present with similar neurological deficits and imaging findings.
- Infections: Brain abscesses, toxoplasmosis (especially in immunocompromised patients), and viral encephalitis can cause lesions that resemble PCNSL on imaging.
- Inflammatory and Demyelinating Diseases: Conditions like multiple sclerosis or sarcoidosis can produce brain lesions that may be confused with PCNSL.
- Ischemic or Hemorrhagic Strokes: Acute neurological deficits can sometimes initially be mistaken for stroke, although imaging usually clarifies this distinction.
Because of these overlaps, a definitive diagnosis almost always requires a biopsy. Relying solely on imaging or clinical presentation can be misleading. The expertise of a multidisciplinary team, including neurologists, radiologists, and neuropathologists, is essential to navigate these diagnostic complexities and ensure accurate identification of PCNSL.
The Critical Role of Early Detection
The aggressive nature of PCNSL underscores the paramount importance of Early detection primary CNS lymphoma. Prompt and accurate diagnosis significantly impacts treatment outcomes and patient prognosis. PCNSL can progress rapidly, and delays in diagnosis can lead to more extensive neurological damage and a reduced window for effective intervention.
When PCNSL is identified early, before significant tumor burden or widespread dissemination within the CNS, patients are often candidates for more effective and less intensive treatment regimens. This can include high-dose chemotherapy, sometimes followed by stem cell rescue, and in select cases, radiation therapy. Early intervention can lead to better disease control, longer progression-free survival, and improved quality of life.
Conversely, delayed diagnosis can result in more advanced disease, making treatment more challenging and potentially requiring more aggressive therapies with greater side effects. It also increases the risk of irreversible neurological deficits. Therefore, a high index of suspicion, especially in at-risk individuals presenting with new or worsening neurological symptoms, is vital for improving the outlook for those affected by this rare but serious condition.
Frequently Asked Questions
What are the first signs of primary CNS lymphoma?
The first signs of primary CNS lymphoma are often non-specific and can include persistent headaches, new-onset seizures, or focal neurological deficits like weakness or vision changes. Patients may also experience cognitive and behavioral changes such as memory loss, confusion, or personality shifts. These symptoms typically develop gradually over weeks to months, making early recognition challenging but crucial for prompt medical evaluation.
How is primary CNS lymphoma definitively diagnosed?
Primary CNS lymphoma is definitively diagnosed through a combination of advanced imaging and pathological confirmation. An MRI with contrast is typically the initial imaging study. The conclusive diagnosis, however, relies on a stereotactic brain biopsy, where a tissue sample is taken from the lesion for microscopic examination. Cerebrospinal fluid analysis via lumbar puncture is also critical to check for malignant cells and assess disease spread.
Are there screening tests for primary CNS lymphoma?
Currently, there are no routine screening tests for primary CNS lymphoma in the general population due to its rarity. Screening efforts are primarily focused on high-risk individuals, such as those with HIV/AIDS or organ transplant recipients on immunosuppressive therapy. For these groups, a heightened awareness and prompt investigation of any new neurological symptoms serve as a form of targeted surveillance rather than broad, population-wide screening.
“`
Diagnosis, Screening, and Early Detection of Primary CNS Lymphoma
Primary Central Nervous System Lymphoma (PCNSL) is a rare and aggressive form of non-Hodgkin lymphoma that originates in the brain, spinal cord, or eyes. Understanding its diagnosis, screening, and the critical importance of early detection is paramount for effective management and improved patient outcomes.
Key Takeaways
- Early detection primary CNS lymphoma is crucial for improving patient prognosis and treatment efficacy.
- Initial symptoms of PCNSL are often non-specific, including neurological deficits and cognitive changes, making diagnosis challenging.
- Primary CNS lymphoma diagnosis methods rely on advanced imaging (MRI) and definitive tissue biopsy or cerebrospinal fluid analysis.
- Universal primary cns lymphoma screening is not standard; screening efforts focus on high-risk populations, such as immunocompromised individuals.
- Differentiating PCNSL from other neurological conditions requires a comprehensive diagnostic approach due to overlapping symptoms and imaging findings.
Recognizing Early Indicators of Primary CNS Lymphoma
Recognizing the Symptoms and early signs of CNS lymphoma is often challenging due to their non-specific nature, frequently mimicking other neurological conditions. These indicators typically develop over weeks to months, making prompt medical evaluation essential.
Common Neurological Symptoms
Patients with PCNSL often present with a range of neurological symptoms that reflect the location and size of the tumor within the central nervous system. These can include:
- Headaches: Persistent or worsening headaches are a common complaint, though they are also associated with many other conditions.
- Seizures: New-onset seizures, either focal or generalized, can be an early indicator, particularly if there’s no prior history of epilepsy.
- Focal Neurological Deficits: Weakness or numbness on one side of the body, visual disturbances (such as blurred vision or double vision), speech difficulties (aphasia), or problems with coordination and balance. These deficits depend on the specific brain region affected.
Cognitive and Behavioral Changes
Beyond physical symptoms, PCNSL can also manifest through subtle yet significant changes in cognitive function and behavior. These changes are often insidious and may initially be attributed to other factors, delaying the Early detection primary CNS lymphoma.
- Memory Loss: Difficulty recalling recent events or learning new information.
- Personality Changes: Increased irritability, apathy, or changes in mood and behavior that are uncharacteristic for the individual.
- Confusion and Disorientation: Problems with concentration, difficulty performing routine tasks, or general confusion about time and place.
According to the National Cancer Institute, these neurological and cognitive symptoms are present in over 70% of PCNSL patients at diagnosis, underscoring the importance of thorough investigation when such signs emerge, especially in at-risk individuals.
Primary CNS Lymphoma Diagnosis Methods
A definitive primary cns lymphoma diagnosis requires a combination of advanced imaging and pathological confirmation. The diagnostic process is crucial for distinguishing PCNSL from other brain lesions and initiating appropriate treatment.
Advanced Imaging Techniques (MRI, CT)
Initial evaluation for suspected PCNSL typically begins with neuroimaging. Magnetic Resonance Imaging (MRI) with contrast is considered the most sensitive imaging modality for detecting brain lesions associated with PCNSL. It can reveal characteristic features such as periventricular lesions, often with homogeneous enhancement after contrast administration.
Computed Tomography (CT) scans may also be used, particularly in emergency settings, but they are generally less sensitive than MRI for detecting subtle lesions. Both techniques help in identifying the location and extent of the tumor, guiding subsequent diagnostic steps. Understanding primary CNS lymphoma diagnosis often starts with these visual clues, though they are not conclusive on their own.
Biopsy and Cerebrospinal Fluid Analysis
The gold standard for confirming a primary cns lymphoma diagnosis is histological examination of tissue. This is typically achieved through a stereotactic brain biopsy, where a small sample of the suspicious lesion is surgically removed and analyzed by a neuropathologist. This procedure allows for definitive identification of lymphoma cells and classification of the specific type of lymphoma.
Cerebrospinal fluid (CSF) analysis is another vital component of the diagnostic workup. A lumbar puncture is performed to collect CSF, which is then examined for the presence of malignant cells (cytology), elevated protein levels, and specific markers via flow cytometry or molecular studies. CSF analysis is particularly important for detecting leptomeningeal involvement, which can impact staging and treatment decisions. These are among the key Primary CNS lymphoma diagnosis methods.
In some cases, especially when brain biopsy is not feasible or safe, vitreous biopsy (for ocular lymphoma) or even bone marrow biopsy might be considered if systemic lymphoma is suspected to rule out secondary CNS involvement.
Screening for Primary CNS Lymphoma
Unlike some more common cancers, there are no universal Screening guidelines for CNS lymphoma for the general population. This is primarily due to the rarity of the disease and the lack of cost-effective, non-invasive screening tests that could identify PCNSL before symptoms appear.
Current Screening Approaches
Currently, there isn’t a standardized or routine primary cns lymphoma screening program. The focus remains on prompt investigation of individuals presenting with suggestive neurological symptoms. Research is ongoing into potential biomarkers in blood or CSF that could indicate the presence of PCNSL, but these are not yet part of routine clinical practice for screening purposes. Therefore, the concept of Best screening tests for CNS lymphoma is largely theoretical for the general public.
Target Populations for Screening
While universal screening is not practical, certain populations are at a higher risk for developing PCNSL, making vigilance and a lower threshold for diagnostic investigation crucial. These target populations include:
- Immunocompromised Individuals: People with HIV/AIDS, particularly those with low CD4 counts, have a significantly increased risk of PCNSL. For this group, any new neurological symptom warrants immediate and thorough investigation.
- Organ Transplant Recipients: Patients on long-term immunosuppressive therapy following organ transplantation also have an elevated risk. Regular monitoring and prompt evaluation of neurological changes are critical.
- Individuals with Primary Immunodeficiency Syndromes: Certain rare genetic conditions that compromise the immune system can also increase PCNSL risk.
For these high-risk groups, clinicians maintain a heightened awareness, and diagnostic imaging or CSF analysis may be performed more readily when symptoms arise, effectively serving as a form of targeted surveillance rather than broad screening.
Differentiating PCNSL from Other Conditions
One of the significant challenges in achieving a timely primary cns lymphoma diagnosis lies in its differentiation from a myriad of other neurological conditions. The symptoms and imaging characteristics of PCNSL can often mimic those of more common diseases, leading to potential delays in diagnosis.
Challenges in Differential Diagnosis
The non-specific nature of PCNSL symptoms means they can overlap with those of various other conditions, including:
- Other Brain Tumors: Gliomas, metastases from systemic cancers, and other primary brain tumors can present with similar neurological deficits and imaging findings.
- Infections: Brain abscesses, toxoplasmosis (especially in immunocompromised patients), and viral encephalitis can cause lesions that resemble PCNSL on imaging.
- Inflammatory and Demyelinating Diseases: Conditions like multiple sclerosis or sarcoidosis can produce brain lesions that may be confused with PCNSL.
- Ischemic or Hemorrhagic Strokes: Acute neurological deficits can sometimes initially be mistaken for stroke, although imaging usually clarifies this distinction.
Because of these overlaps, a definitive diagnosis almost always requires a biopsy. Relying solely on imaging or clinical presentation can be misleading. The expertise of a multidisciplinary team, including neurologists, radiologists, and neuropathologists, is essential to navigate these diagnostic complexities and ensure accurate identification of PCNSL.
The Critical Role of Early Detection
The aggressive nature of PCNSL underscores the paramount importance of Early detection primary CNS lymphoma. Prompt and accurate diagnosis significantly impacts treatment outcomes and patient prognosis. PCNSL can progress rapidly, and delays in diagnosis can lead to more extensive neurological damage and a reduced window for effective intervention.
When PCNSL is identified early, before significant tumor burden or widespread dissemination within the CNS, patients are often candidates for more effective and less intensive treatment regimens. This can include high-dose chemotherapy, sometimes followed by stem cell rescue, and in select cases, radiation therapy. Early intervention can lead to better disease control, longer progression-free survival, and improved quality of life.
Conversely, delayed diagnosis can result in more advanced disease, making treatment more challenging and potentially requiring more aggressive therapies with greater side effects. It also increases the risk of irreversible neurological deficits. Therefore, a high index of suspicion, especially in at-risk individuals presenting with new or worsening neurological symptoms, is vital for improving the outlook for those affected by this rare but serious condition.
Frequently Asked Questions
What are the first signs of primary CNS lymphoma?
The first signs of primary CNS lymphoma are often non-specific and can include persistent headaches, new-onset seizures, or focal neurological deficits like weakness or vision changes. Patients may also experience cognitive and behavioral changes such as memory loss, confusion, or personality shifts. These symptoms typically develop gradually over weeks to months, making early recognition challenging but crucial for prompt medical evaluation.
How is primary CNS lymphoma definitively diagnosed?
Primary CNS lymphoma is definitively diagnosed through a combination of advanced imaging and pathological confirmation. An MRI with contrast is typically the initial imaging study. The conclusive diagnosis, however, relies on a stereotactic brain biopsy, where a tissue sample is taken from the lesion for microscopic examination. Cerebrospinal fluid analysis via lumbar puncture is also critical to check for malignant cells and assess disease spread.
Are there screening tests for primary CNS lymphoma?
Currently, there are no routine screening tests for primary CNS lymphoma in the general population due to its rarity. Screening efforts are primarily focused on high-risk individuals, such as those with HIV/AIDS or organ transplant recipients on immunosuppressive therapy. For these groups, a heightened awareness and prompt investigation of any new neurological symptoms serve as a form of targeted surveillance rather than broad, population-wide screening.
