Revolutionary ChatGPT-Powered Chatbot Platform
AskFiona AI & DrArturo AI
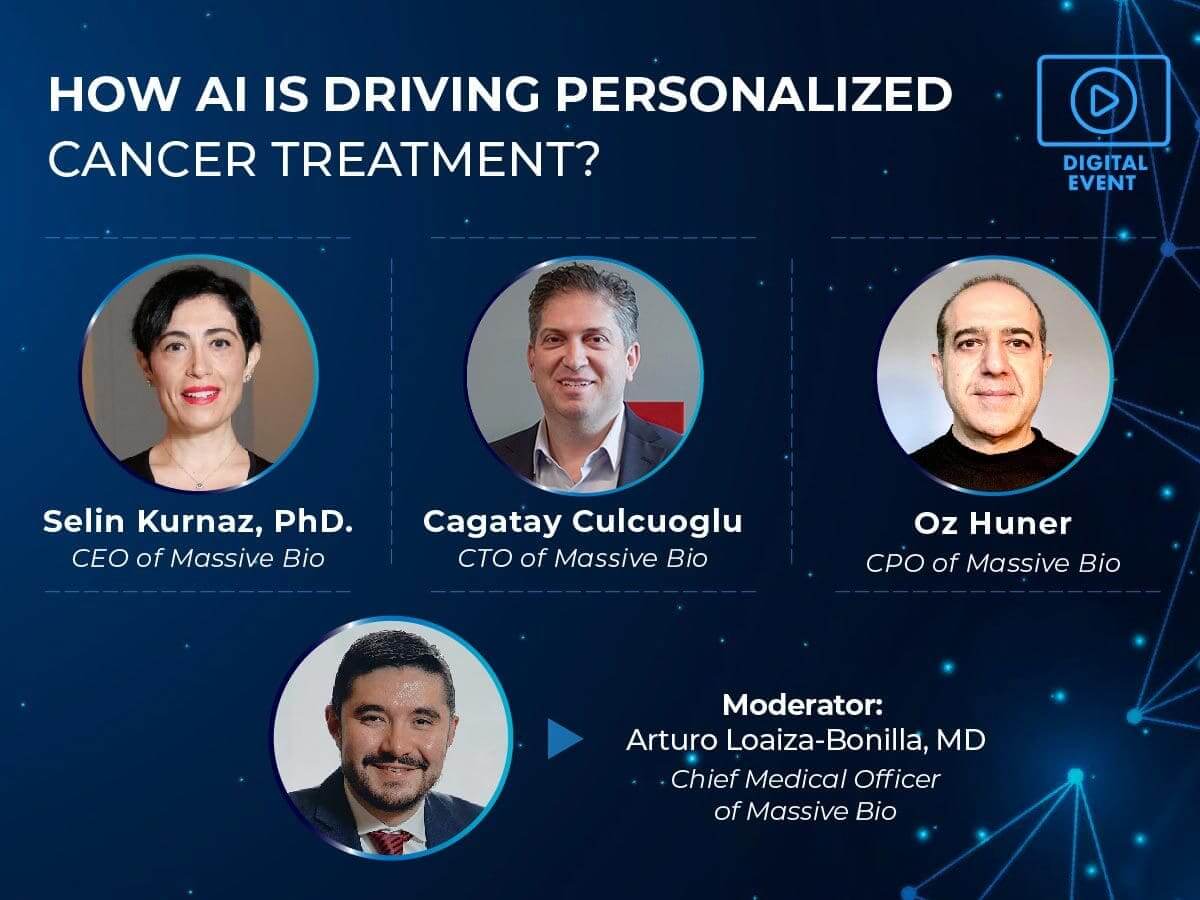
Massive Bio, a world-renowned provider of personalized oncology solutions, is set to showcase its groundbreaking GPT4 AI chatbots - AskFiona AI and DrArturo. These innovative, AI-driven solutions will redefine cancer care, establishing new paradigms in patient and provider engagement and global oncological research. Massive Bio's ChatGPT-powered platform lies at the heart of the transformation in clinical trials. Incorporating AskFiona AI and DrArturo AI will transcend the capabilities of Massive Bio's existing SYNERGY-AI Clinical Trial Matching Solution, thereby heralding a new epoch in personalized oncology solutions.
Services we provide
a disease. Clinical trials can also be used to learn if a new treatment is more effective
or has less harmful side effects than the standard treatment.
A board of physicians make expert recommendations on your best course of treatment.
We coordinate with your local physician and facilitate the process of implementing the recommendations locally.
We track your progress and are with you every step of the way.
You’ll have access to the Massive Bio social media community of team members and other patients who’ve gone through the process.
Clinical Trial Enrollment
We believe patients need to be fully informed of all of their options, including the opportunity to enroll in clinical trials.
More details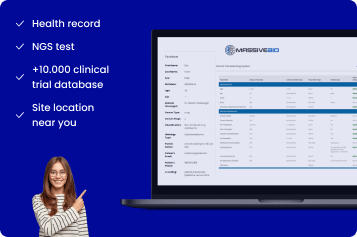
Solutions
Learn more about Massive Bio B2B services
successful treatments
successful treatments
Cancer is a word that everyone cringes at. You need services like Massive Bio to keep hope and possible alternatives when doors seem to close. The amount of education is phenomenal, and the staff was very compassionate. I would recommend the services for those seeking that alternative to “Standardized treatment”, not everyone can handle them.
With my recent progession on Lorlatinib, I've been working hard to find a clinical trial that I may fit into. It has not been easy. I am so lucky that recently, I talked to a company that helps people like me. If you register, they will connect you with a clinical trial-even if you don't have progression.
So far, my experience with Massive Bio has been very positive. My initial interaction with Eric was informative and he provide me with the proper forms to be completed. The initial report and clinical trial recommendations was excellent. The report provided a details summary of my complete cancer medical history including test results, chemotherapy treatments (which revealed an error in the history on file at one medical institution), and procedures. My follow up conversation with Kristin Johnston was professional, informative and educational. She spent a lot of time with me reviewing the clinical trial options, answering my questions on my current chemotherapy treatment regiment, and was proactive regarding follow up and next steps. I look forward to working with Massive Bio on my current cancer journey and hope that they can assist me with combatting and winning this battle. Best partner for cancer.
My experience with Massive Bio was professional and satisfying. As a stage 4 cancer patient seeking a second opinion and treatment plan due to recurrence of a stomach tumor, I did not have time to lose negotiating the customary hurdles of my HMO insurance plan. I needed to quickly get opinions of recognized leaders in the field. The concept of a Virtual Tumor Board with quality doctors and health care professionals affiliated with Massive Bio was appealing. I was convinced this approach was worth a try...and I was not disappointed. After meticulously collecting details about past diagnoses, treatments, and tests, a thorough report was submitted to both me and my primary oncologist within days. The treatment plan prioritized strategies and reviewed clinical trials appropriate to my case. The plan was so thorough, well conceptualized, and clearly written that my oncologist and I had only a few questions. Those that we did raise were answered quickly and concisely.
Massive Bio worked in collaboration with my local treating oncologist to analyze my carcinoma based on my personal cancer treatment information. In one week, Massive Bio's Virtual Tumor Board experts provided valuable insight and an informative medical report to my doctor. Collaboratively, we agreed that the clinical trial Massive Bio identified was the best option to move ahead.

Patient - United States of America - February 2021

Patient – United States of America – September 2020

Patient – United States of America – June 2020

Patient – United States of America – January 2019

Patient - United States of America - March 2018

Patient - United States of America - February 2017




































Massive Bio preformed a vital role in my acceptance into the clinical trial. There were times when I felt Massive Bio was the only champion I had working toward my acceptance into the clinical trial!